Pilates for Prolapse: Strengthening Your Core Safely and Effectively
Share
Prolapse refers to the dropping or sliding of an organ from its normal position. It typically occurs in pelvic organs like the bladder, uterus, or rectum. The condition is most commonly seen in women, especially after childbirth or menopause, but it can occur in men too (though less frequently). Prolapse occurs when the muscles and tissues supporting these organs become weak or stretched, leading to the organs shifting downward into the vaginal or rectal canal.
Types of Prolapse
- Pelvic Organ Prolapse (POP): Includes conditions like uterine prolapse, cystocele (bladder prolapse), and rectocele (rectal prolapse).
- Urethral Prolapse: The urethra (the tube that carries urine from the bladder) prolapses or drops out of its usual position.
Symptoms of Prolapse
- A feeling of heaviness or pressure in the pelvic area
- The sensation of something "falling out" or a bulge in the vagina or rectum
- Urinary issues, like incontinence or difficulty emptying the bladder
Pelvic Organ Prolapse (POP) is a condition where one or more of the pelvic organs (bladder, uterus, rectum, or small bowel) drop or bulge into the vaginal or rectal canal due to weakened or stretched pelvic floor muscles and connective tissues. This can lead to discomfort, urinary or bowel issues, and a sensation of heaviness or pressure in the pelvic area.
Common Causes of POP:
- Childbirth: Vaginal delivery, especially with multiple births or large babies, can stretch and weaken the pelvic floor muscles.
- Aging: As women age, particularly after menopause, the decrease in estrogen levels can weaken pelvic tissues, increasing the risk of prolapse.
- Chronic Constipation: Straining during bowel movements can place pressure on the pelvic floor muscles over time.
- Obesity: Excess body weight increases pressure on the pelvic floor, contributing to the weakening of supporting tissues.
- Heavy Lifting: Repeated heavy lifting can strain the pelvic floor and lead to prolapse.
- Genetics: Some women may be more prone to POP due to inherited connective tissue weaknesses.
- Hysterectomy: Surgical removal of the uterus can weaken pelvic structures and lead to prolapse of other organs.
How Exercise Affects Prolapse
Exercise can play an important role in managing prolapse. However, it's important to approach exercise carefully and with the right guidance. Some exercises can help strengthen the pelvic floor muscles, while others may exacerbate prolapse if done incorrectly.
Beneficial Exercises for Prolapse
-
Pelvic Floor Exercises (Kegels): Strengthening the pelvic floor muscles can help provide better support to the organs and prevent further prolapse. Kegels involve contracting and relaxing the pelvic muscles that control urination, bowel movements, and sexual function.
- How to do them: Contract your pelvic floor muscles as if you're gently stopping the flow of urine or holding back gas. Hold the contraction for a few seconds, then relax. Gradually increase the duration and repetitions.
-
Core Strengthening: Strengthening the core (abdominals, back, and pelvis) can improve posture and support the pelvic floor. Examples include:
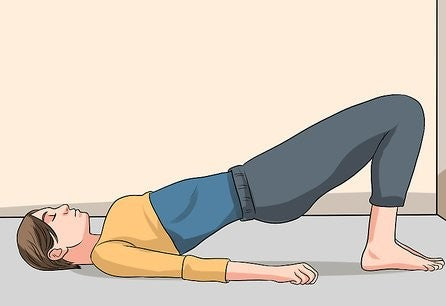
- Bridges: Lying on your back with knees bent, lift your hips toward the ceiling while squeezing the glutes and engaging the core.
- Bird-dog: On all fours, extend one arm forward and the opposite leg back, while engaging your core to maintain stability.
-
Breathing Techniques: Diaphragmatic breathing or pelvic floor breathing can help relax and strengthen the pelvic floor muscles. Focus on expanding the diaphragm fully while gently engaging the pelvic floor muscles with each exhale.
-
Postural Awareness: Improving posture, especially when standing, sitting, or lifting, can alleviate pressure on the pelvic organs and promote proper alignment.
Exercises to Avoid with Prolapse
Some exercises may put too much strain on the pelvic floor, leading to worsening symptoms. It's generally recommended to avoid or modify:
- Heavy lifting or lifting with improper form: This can increase intra-abdominal pressure, which may exacerbate prolapse.
- High-impact activities (running, jumping): These can increase pressure on the pelvic floor.
- Crunches or sit-ups: These exercises can engage the abdominal muscles in a way that increases pressure on the pelvic area, potentially worsening prolapse symptoms.
- Squats or lunges (without proper pelvic floor engagement): These exercises, if done incorrectly, can place undue strain on the pelvic floor.
Guidelines for Safe Exercise with Prolapse
-
Work with a Professional: If you have prolapse, it's a good idea to work with a pelvic health physiotherapist or trainer experienced with prolapse. They can design a program tailored to your needs and limitations.
-
Focus on Low-Impact Activities: Walking, swimming, and gentle yoga can help improve overall fitness without adding excessive strain to the pelvic region.
-
Mind Your Posture: Proper posture helps reduce pressure on the pelvic floor during exercise. When lifting, always ensure you’re engaging your pelvic floor and core muscles.
-
Don’t Push Through Pain: If you experience any discomfort or pressure during exercise, stop and consult a healthcare professional. Exercise should never cause pain or exacerbate prolapse symptoms.
-
Gradual Progression: Start slowly and gradually increase the intensity or duration of exercises. Overexertion can worsen prolapse symptoms.
If you suspect prolapse, it’s important to consult with a pelvic health expert or doctor who can guide you on the best exercise plan based on your condition.
Pilates, when done correctly, can be a highly effective way to support pelvic health and aid in recovery from conditions like pelvic organ prolapse (POP), pelvic floor dysfunction, or after childbirth. The key lies in targeting the pelvic floor muscles, improving core strength, and enhancing overall body awareness. Here's how Pilates can support pelvic health:
1. Strengthening the Pelvic Floor
Pilates emphasizes controlled, mindful movements that engage the pelvic floor muscles, which are crucial for supporting the pelvic organs. Exercises like pelvic floor contractions (similar to Kegels) help strengthen these muscles, providing better support and stability for the bladder, uterus, and rectum. Regular engagement of the pelvic floor can reduce the risk of prolapse and help manage mild symptoms.
2. Improving Core Strength
A strong core (including the deep abdominal muscles, lower back, and pelvic floor) is central to Pilates. Many Pilates exercises focus on strengthening the transverse abdominis and the multifidus muscles, which help support the spine and pelvis. A strong core improves posture and reduces strain on the pelvic floor, promoting better function and reducing the risk of prolapse or pelvic pain.
3. Promoting Proper Alignment and Posture
Pilates places a significant emphasis on body alignment and posture. Correct posture minimizes pressure on the pelvic region, which is especially important for individuals with prolapse or pelvic floor issues. By improving posture, Pilates helps redistribute weight and reduce unnecessary strain on the pelvic organs, preventing further damage.
4. Enhancing Body Awareness
Pilates encourages mindfulness and awareness of how the body moves, including how the pelvic floor and core engage during exercises. This increased awareness can help individuals better manage pelvic health in daily activities, improving posture, breathing, and movement patterns. It's particularly helpful for avoiding activities that could strain the pelvic floor, such as heavy lifting or incorrect body mechanics during physical tasks.
5. Encouraging Controlled Breathing
Proper breathing techniques are integral to Pilates practice. The focus on diaphragmatic breathing (deep breathing into the diaphragm) helps reduce intra-abdominal pressure, which can otherwise contribute to pelvic floor stress. By using the breath effectively, Pilates helps maintain a healthy balance between muscle engagement and relaxation, promoting pelvic floor recovery and function.
6. Rehabilitating After Childbirth
Pilates can be especially beneficial for postnatal recovery, as it helps rebuild strength in the pelvic floor and abdominal muscles after the strain of pregnancy and childbirth. Exercises that focus on pelvic floor activation and core strengthening can support healing, reduce the risk of prolapse, and restore functionality to the pelvic region.
7. Low-Impact, Gentle Movements
Pilates is a low-impact form of exercise, making it ideal for those with pelvic floor issues or prolapse. It avoids high-impact movements (like running or jumping) that could put excessive pressure on the pelvic region. Instead, Pilates focuses on slow, controlled movements that strengthen muscles without overstretching or causing injury.
Key Pilates Exercises for Pelvic Health
- Pelvic Tilts: Help strengthen the pelvic floor while improving spinal alignment.
- Bridges: Strengthen the glutes, core, and pelvic floor muscles, supporting pelvic stability.
- Cat-Cow Stretch: Promotes spinal mobility and engages the pelvic floor muscles.
- Dead Bug: Strengthens core muscles while encouraging proper pelvic positioning.
- Leg Slides: Strengthen the lower abdominal muscles and engage the pelvic floor.
When practiced with proper technique and attention to form, Pilates can be an excellent tool for supporting pelvic health, improving pelvic floor strength, and facilitating recovery from conditions like prolapse. However, it’s important to work with a trained Pilates instructor who understands pelvic health, particularly if you’re managing pelvic floor dysfunction or recovering from injury, childbirth, or surgery. They can ensure exercises are adapted to your needs, reducing the risk of exacerbating symptoms and supporting safe, effective recovery.
Pilates plays a significant role in pelvic floor health by providing a safe, effective way to strengthen the muscles that support the pelvic organs (bladder, uterus, rectum, etc.) and improve overall pelvic function. The pelvic floor muscles are crucial for bladder and bowel control, sexual function, and supporting the pelvic organs. Pilates, with its focus on controlled movement, alignment, and core engagement, can be a powerful tool for maintaining and improving pelvic floor health. Here's how Pilates supports pelvic floor function:
1. Strengthening the Pelvic Floor Muscles
One of the core benefits of Pilates for pelvic health is its ability to target and strengthen the pelvic floor muscles. Pilates exercises that emphasize core engagement (like pelvic tilts, bridges, or certain breathwork techniques) work the pelvic floor in conjunction with the deeper abdominal muscles. This helps improve muscle tone and strength in the pelvic region, which can prevent or manage conditions like pelvic organ prolapse, urinary incontinence, and pelvic pain.
2. Improving Core Stability and Alignment
Pilates places a strong emphasis on the deep core muscles, including the transverse abdominis, diaphragm, and multifidus (a deep back muscle), all of which support the pelvic floor. A strong core helps to stabilize the pelvis and relieve unnecessary pressure on the pelvic floor. Proper alignment in Pilates also helps individuals engage the pelvic floor muscles more effectively during exercises, improving pelvic function.
3. Enhancing Pelvic Floor Awareness
Pilates encourages mind-body connection and awareness, which can help people develop better control over their pelvic floor muscles. Many Pilates exercises involve mindful breathing and pelvic floor engagement, helping individuals become more conscious of how their pelvic muscles work during movement. This increased awareness can lead to better pelvic floor activation and relaxation in daily activities, improving overall pelvic health.
4. Breathing Techniques and Pelvic Floor Relaxation
Pilates integrates diaphragmatic (deep) breathing, which helps reduce intra-abdominal pressure and can improve pelvic floor relaxation. Breathing properly while engaging the core muscles during Pilates helps to coordinate the contraction and relaxation of the pelvic floor muscles. This is especially important for people experiencing pelvic floor tension or over-activity, as it encourages the pelvic muscles to release and relax.
5. Improving Posture and Reducing Pressure on the Pelvic Floor
Proper posture is a central element in Pilates. By learning to maintain a neutral spine and correct pelvic alignment, individuals can reduce pressure on the pelvic floor that might result from poor posture. For example, slouching or leaning forward during movement can increase pressure on the pelvic floor, while proper alignment helps maintain an optimal balance between muscle engagement and relaxation.
6. Rehabilitation and Recovery
Pilates is often used in rehabilitation programs for those recovering from pelvic floor dysfunction, childbirth, or pelvic surgeries. Postnatal Pilates, in particular, can help women regain pelvic floor strength and address any pelvic floor issues caused by pregnancy or delivery. For people with conditions like pelvic organ prolapse or incontinence, Pilates can offer a safe and gentle way to restore muscle tone and prevent further deterioration.
7. Low-Impact Exercise for Pelvic Floor Health
Pilates is a low-impact form of exercise, which makes it ideal for individuals with pelvic floor issues. Unlike high-impact activities (running, jumping), which can strain the pelvic floor muscles and worsen symptoms, Pilates offers controlled, mindful movements that allow individuals to safely strengthen the pelvic floor without causing excessive pressure or strain.
Key Pilates Exercises for Pelvic Floor Health:
- Pelvic Tilts: Help activate and strengthen the pelvic floor muscles, improving alignment.
- Bridges: Strengthen the glutes, hamstrings, and pelvic floor muscles while maintaining pelvic stability.
- Cat-Cow Stretch: Mobilizes the spine and engages the pelvic floor muscles, promoting better body awareness.
- Dead Bug: Strengthens the core while engaging the pelvic floor and stabilizing the pelvis.
- Knee Folds: Engage the lower abdominals and pelvic floor muscles, encouraging pelvic stability and control.
Incorporating Pilates into your routine can be an effective way to maintain and improve pelvic floor health. By focusing on strengthening the pelvic floor muscles, improving core stability, and promoting better posture and body awareness, Pilates can help prevent pelvic floor dysfunction, support recovery from pelvic conditions, and improve overall pelvic health.
For those with existing pelvic floor issues, it’s essential to work with a trained Pilates instructor who is knowledgeable about pelvic health to ensure that exercises are safe and appropriately modified to address individual needs. This personalized approach will maximize the benefits of Pilates for pelvic floor health and overall well-being.
Postural adjustments are key for reducing pressure on the pelvic floor, especially for individuals dealing with pelvic floor dysfunction, prolapse, or other pelvic health concerns. Proper alignment and body mechanics help prevent excessive strain on the pelvic floor muscles and support optimal pelvic health. Here are some key postural adjustments that can reduce pressure on the pelvic floor:
1. Maintain a Neutral Spine
The neutral spine position is crucial for reducing pelvic floor pressure. A neutral spine is the natural curve of the spine, where the lower back (lumbar) has a slight inward curve, the mid-back (thoracic) curves outward, and the neck (cervical) curves inward. When standing, sitting, or moving, try to maintain this alignment to avoid over-arching or slumping, which can increase pressure on the pelvic floor.
- How to do it: Imagine a string pulling you upward from the crown of your head. Engage your core slightly and avoid excessive sway in your lower back (lumbar spine). Keep your pelvis in a neutral position—not tilting forward or backward.
2. Avoid Excessive Anterior Pelvic Tilt
An anterior pelvic tilt (when the pelvis tilts forward, creating an exaggerated curve in the lower back) increases pressure on the pelvic floor. This posture often results in a “swayback” or arched lower back, which can put undue strain on pelvic organs.
- How to correct it: Stand with your feet hip-width apart and your weight evenly distributed. Engage your glutes and slightly tuck your pelvis under to bring it into a more neutral position, avoiding the excessive arching of your lower back.
3. Use Proper Sitting Posture
When sitting, especially for long periods, it’s important to maintain a neutral spine and avoid slouching, which can increase pressure on the pelvic floor. Slouching or leaning forward in the chair can push the pelvis out of alignment, straining the pelvic region.
- How to sit correctly: Sit upright with your feet flat on the floor and your knees at a right angle. Keep your spine aligned (no slumping), and avoid crossing your legs for long periods. Sit on the sit bones (ischial tuberosities) rather than on your tailbone to reduce pressure on the pelvic floor.
4. Engage the Core and Pelvic Floor
Whether standing, sitting, or moving, gently engage your core muscles (abdominals, back muscles) and pelvic floor muscles to create internal support. This will help reduce pressure on the pelvic floor by redistributing forces through the torso and reducing the strain on the pelvic region.
- How to engage: Draw your lower belly gently inward (not holding your breath or sucking in) and lift the pelvic floor muscles (as if you’re stopping the flow of urine). Practice engaging your pelvic floor and core muscles throughout daily activities.
5. Correct Lifting Mechanics
Lifting objects improperly, such as bending at the waist or twisting, can increase pressure on the pelvic floor. Proper lifting techniques are crucial for minimizing strain.
- How to lift correctly: When picking something up, bend at the hips and knees rather than at the waist. Engage your core and pelvic floor as you squat down to pick up the object. Keep the object close to your body and lift using your legs, not your back.
6. Stand with a Balanced Weight Distribution
When standing for long periods, uneven weight distribution can create an imbalance in your posture, leading to unnecessary pressure on the pelvic floor.
- How to stand properly: Distribute your weight evenly between both legs. Avoid locking your knees or shifting weight to one side. Imagine a straight line running from the top of your head down through your pelvis and to your feet. Stay aligned and avoid hyper-extending your knees.
7. Mindful Breathing
Breathing techniques are essential for pelvic floor health, as improper breathing can create additional intra-abdominal pressure, which increases stress on the pelvic region.
- How to breathe correctly: Practice lLATERAL THORACIC BREATHING-diaphragmatic breathing—breathe deeply into your diaphragm, letting your belly expand as you inhale, and then gently contract as you exhale. This type of breathing encourages pelvic floor relaxation and helps prevent pressure buildup.
8. Engage the Glutes and Hamstrings
When standing, sitting, or walking, engaging the glutes and hamstrings can provide additional support to the pelvic region and reduce pressure on the pelvic floor muscles.
- How to engage: When standing or walking, imagine slightly pulling your glutes together as if you were trying to lift them. This engagement helps stabilize the pelvis and support the pelvic floor.
9. Avoid Holding the Breath
Holding your breath (especially during exertion or lifting) increases intra-abdominal pressure, which can exacerbate pelvic floor dysfunction or prolapse. Exhalation during exertion helps keep pressure balanced.
- How to breathe during exertion: When lifting, squatting, or exerting yourself, exhale as you perform the effort (e.g., lifting, pushing). This helps to lower intra-abdominal pressure and protect the pelvic floor.
10. Proper Foot Alignment
The position of your feet can affect your overall posture and alignment, which in turn impacts pelvic floor pressure. Misalignment of the feet or lower legs can lead to compensatory movements that put stress on the pelvic area.
- How to align your feet: When standing, keep your feet hip-width apart with toes pointing forward (not turned out or in). Ensure your knees are aligned with your toes, avoiding any inward or outward rotation that could shift your pelvis out of alignment.
Correct posture and body mechanics are key to supporting the pelvic floor and reducing unnecessary pressure. Being mindful of how you sit, stand, lift, and move throughout the day can help preserve pelvic health and prevent pelvic floor dysfunction. Pilates, with its focus on alignment, core engagement, and mindful movement, can be a helpful way to reinforce these postural adjustments.
Supporting pelvic floor health is an important aspect of overall well-being, and adopting healthy lifestyle habits can play a crucial role in maintaining or improving pelvic floor function. Hydration, nutrition, and other lifestyle choices can either help or hinder the strength and function of the pelvic floor muscles, which support the pelvic organs and contribute to bladder, bowel, and sexual health. Here's a look at lifestyle tips that promote pelvic floor health, with a focus on hydration and nutrition:
1. Hydration
Staying properly hydrated is essential for the function of all muscles in the body, including the pelvic floor. Dehydration can lead to a range of issues, including urinary problems and muscle weakness.
-
Why hydration matters: Proper hydration helps maintain the elasticity and strength of the pelvic floor muscles. Dehydration can lead to urinary tract infections (UTIs), constipation, and urinary incontinence. Drinking enough water ensures that the body is able to flush out toxins and maintain healthy organ function.
-
How much water to drink: The general recommendation is to drink around 8 cups (64 ounces) of water a day, but this can vary depending on your activity level, age, and health conditions. For optimal pelvic health, aim to drink enough to keep your urine light yellow, as dark urine can indicate dehydration.
-
Balancing hydration: While drinking plenty of water is important, also avoid excessive consumption of caffeinated or alcoholic beverages, as they can irritate the bladder and contribute to increased urgency or frequency of urination. If you're prone to bladder issues, try to limit drinks like coffee, soda, or alcohol, which can act as diuretics.
2. Nutrition
What you eat plays a direct role in maintaining pelvic floor health. A well-balanced diet can support muscle strength, digestive health, and hormonal balance—all of which affect the pelvic region.
Fiber-Rich Foods (Prevent Constipation)
Constipation can place significant strain on the pelvic floor muscles, as straining during bowel movements increases intra-abdominal pressure and may contribute to prolapse or pelvic floor dysfunction.
-
Why fiber is important: Fiber helps promote regular bowel movements and prevents constipation by softening stool and making it easier to pass. This reduces the need for excessive straining during bowel movements, which can stress the pelvic floor.
-
Foods to include: Whole grains (brown rice, oats, quinoa), legumes (beans, lentils), fruits (apples, berries, pears), vegetables (broccoli, spinach, carrots), and nuts and seeds (chia seeds, almonds) are all excellent sources of fiber.
-
How much fiber: Aim for 25-30 grams of fiber per day, which is recommended for most adults to support regular bowel movements and reduce the risk of pelvic floor strain.
Maintain a Healthy Weight
Being overweight or obese increases pressure on the pelvic floor, which can lead to muscle weakness and contribute to prolapse, incontinence, and other pelvic health issues.
-
Why weight management matters: Excess body weight can weaken the pelvic floor muscles over time, contributing to pelvic organ prolapse or urinary incontinence. Maintaining a healthy weight through balanced nutrition can reduce excess pressure on the pelvic area and support overall pelvic health.
-
How to manage weight: Eating nutrient-dense foods (fruits, vegetables, lean proteins, whole grains) while limiting processed foods and refined sugars can help maintain a healthy weight. Pairing a balanced diet with regular physical activity (like Pilates, walking, or swimming) is an effective strategy for weight management.
Protein for Muscle Health
Adequate protein intake is essential for maintaining muscle strength, including the muscles of the pelvic floor. Protein supports tissue repair and helps maintain muscle tone, which is important for pelvic floor function.
-
Why protein is important: Protein helps build and repair muscles, including those that support the pelvic organs. A deficiency in protein can impair muscle function, leading to weakness or dysfunction in the pelvic floor.
-
Sources of protein: Include lean meats (chicken, turkey), fish (salmon, tuna), plant-based options (tofu, tempeh, legumes), eggs, and dairy (Greek yogurt, cottage cheese) in your diet.
Healthy Fats for Hormonal Balance
Hormones play an important role in pelvic floor health, especially for women. Hormonal changes during pregnancy, menopause, and the menstrual cycle can affect the strength and function of the pelvic floor.
-
Why healthy fats matter: Healthy fats, such as omega-3 fatty acids, support hormone production and balance. Imbalanced hormones can weaken pelvic floor muscles, making them more prone to dysfunction.
-
Sources of healthy fats: Include sources of omega-3 fatty acids, such as fatty fish (salmon, mackerel), walnuts, chia seeds, flaxseeds, and olive oil. These fats are also anti-inflammatory, which can help prevent pelvic floor pain or discomfort.
Calcium and Vitamin D for Bone and Muscle Health
Calcium and vitamin D are essential for overall musculoskeletal health, including the muscles of the pelvic floor. Both nutrients play a role in maintaining bone density and muscle function, which can help prevent prolapse and support pelvic health.
-
Why calcium and vitamin D matter: These nutrients help maintain strong bones and muscles. Inadequate levels of calcium or vitamin D can weaken bones and muscles, increasing the risk of pelvic floor issues.
-
Sources of calcium and vitamin D: Calcium-rich foods include dairy products (milk, yogurt, cheese), leafy greens (kale, spinach), and fortified plant-based milks. Vitamin D can be obtained through sunlight exposure, fatty fish, and fortified foods (such as fortified milk and cereals).
3. Avoid Bladder Irritants
Certain foods and drinks can irritate the bladder, which may exacerbate urinary incontinence, frequency, or urgency. Minimizing bladder irritants can help reduce strain on the pelvic floor.
- Bladder irritants to limit or avoid: Caffeine (coffee, tea, soda), alcohol, spicy foods, acidic foods (tomatoes, citrus), and artificial sweeteners can irritate the bladder. If you have issues with bladder control or pelvic floor dysfunction, consider reducing these irritants.
Hydration and nutrition are foundational elements of pelvic floor health. By staying hydrated, eating a fiber-rich diet, maintaining a healthy weight, and including muscle-strengthening foods (like protein and healthy fats), you can support the function and strength of your pelvic floor muscles. A balanced lifestyle, including regular physical activity and mindful movement practices like Pilates, further enhances pelvic health and can prevent or improve pelvic floor dysfunction. If you have specific concerns, it's always a good idea to consult with a healthcare provider or a pelvic health specialist for personalized advice.
Pilates is a Long-Term Solution for Prolapse
You can move safely and feel strong with the right guidance.
